Cervicogenic headache
Cervicogenic Headache
What is Cervicogenic Headache?
Cervicogenic headache (CGH) is a chronic unilateral dull headache with ipsilateral shoulder and arm pain with a restricted range of movements of the neck (1) classified under secondary headache by International Headache Society(IHS). Essentially it is referred pain from certain pathologies of the cervical region.(2)
Epidemiology
It is a rare entity occurring in men and women equally in their early 30’s. It accounts for 1-4% of all headaches. (1)
Types
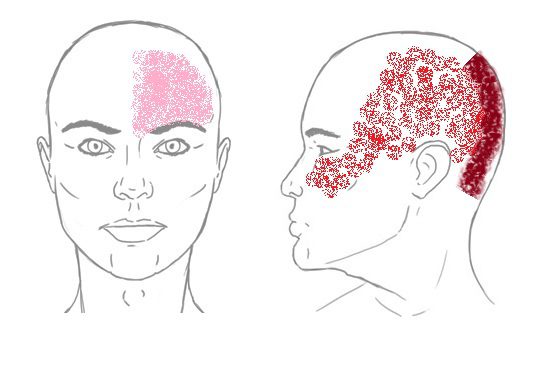
(1) Occipital CGH (2) Occipito-temporo-maxillary CGH and (3) Supra-orbital CGH are the three types of headache based on the region of pain. The three types overlap frequently. (3)
Predisposing factors
- Occupational hazards: Hairstylists, carpenters, drivers, and other occupations that involve abnormal head posture while working may predispose to CGH
- Strenuous activities can produce CGH. Eg: Weight-lifting sportsmen.
- Forward head posture: Holding the head out in a forward position such as working on a computer on a continual basis may pose risk for CGH. (4)
Etiology
Sources of pain:
One or more of the following may be the source of pain in CGH.
- Facet joints
- Atlanto-occipital joint
- Intervertebral discs
- Neck muscles
- Cervical nerves
Causes of pain:
- Trauma: Whiplash injury from rear-end car accidents causing zygo-apophyseal joint injury account for 53% of CGH.(5) Fall or sports injury causing facet joint dislocation, fractures can be other traumatic causes for CGH.
- Inflammatory conditions: Rheumatoid arthritis, Cervical disc disease also produce CGH.
- Degenerative conditions: Cervical degenerative disc disease or osteoarthritis of the facet joints are degenerative causes of CGH.
- Neoplastic conditions: Malignant or benign tumours of the neck can cause compression of the spinal nerves leading to CGH. (4)
Pathophysiology
The trigeminocervical nucleus which receives afferents from the trigeminal nerve and the upper cervical spinal nerves (C1-C3) transmits pain to the trigeminal region of the face through the efferent trigemino-thalamic tract.(1)
Clinical features
Cervicogenic headaches mimic migraines. It is mostly unilataral.
History
- Age group: Early 30’s
- Pain
- Unilateral dominant headache, originates in the neck and radiates to the eye, the temple and the ear.
- Intermittent pain initially which becomes continuous
- Dull ache – mild to moderate in intensity
- Associated features – pain in the ipsilateral shoulder and arm with reduced neck flexibility; blurriness and swelling of the eye.
- Aggravating factors – abnormal postures of neck and neck strain such as pressure on the neck, weight-lifting, coughing and sneezing.
- Relieving factors – local anaesthetic blockade of selective nerve roots
- History of trauma
Examination
- Tenderness over C1-C3 joints
- Spasm and trigger points in upper trapezius, levator scapulae, scales and suboccipital extensors.
- Weakness of the deep flexors of the neck
- Increased activity of the superficial flexors
- Atrophy of the suboccipital extensors
- Flexion-rotation test: The patient should be pain-free at the time of testing. The neck of the patient is passively held in complete flexion followed by rotation of the neck to each side until they feel resistance or until the patient complaints of pain. The range of movement is assessed. The test is considered positive when the estimated range is reduced by 10° or more from the anticipated normal range (44°).
Diagnosis:
The diagnostic criteria are as follows as described by the IHS:
- Any headache fulfilling criterion C
- Clinical, laboratory and/or imaging evidence of a disorder or lesion within the cervical spine or soft tissues of the neck, known to be able to cause headache
- Evidence of causation demonstrated by at least two of the following:
- Headache has developed in temporal relation to the onset of the cervical disorder or appearance of the lesion
- Headache has significantly improved or resolved in parallel with improvement in or resolution of the cervical disorder or lesion
- Cervical range of motion is reduced and headache is made significantly worse by provocative manoeuvres
- Headache is abolished following diagnostic blockade of a cervical structure or its nerve supply
- 5. Not better accounted for by another ICHD-3 diagnosis.(6)
Management
Management is interprofessional involving physical therapists, psychologists and pain specialists. (7–11)
- Physical therapy options
- Cervical spine manipulation or mobilization
- Deep flexor strengthening and upper quarter strengthening exercises
- Thoracic spine thrust manipulation exercises
- C1-C2 Self-sustained Natural Apophyseal Glide(SNAG)
- Trigger point therapy
- Sensorimotor training
- Re-education of posture
- Psychological interventions – Biofeedback, Relaxation and Cognitive behavioural therapy
- Medical pain management
- Tri-cyclic antidepressants: low dose
- Muscle -relaxants
- Botulinum toxin injection : to reduce hypertonia of muscles
- Interventional pain management
- Cervical epidural steroid injections
- Trigger point injections
- Selective nerve root injections
- Radiofrequency thermal neurolysis
Red flags
- Sudden onset severe new headache;
- A worsening pattern of a pre-existing headache without any precipitating factors;
- Headache associated with fever, neck stiffness, skin rash, and with a history of cancer, HIV, or other systemic illness;
- Headache associated with focal neurologic signs other than typical aura;
- Moderate or severe headache triggered by straining; and
- New onset headache during or following pregnancy.
Patients with one or more red flags should be referred for an immediate medical consultation and further investigation. (12)
References
- Cervicogenic Headache [Internet]. Physiopedia. [cited 2020 Oct 2]. Available from: https://www.physio-pedia.com/Cervicogenic_Headache
- DO ZM. What Is Cervicogenic Headache? [Internet]. Spine-health. [cited 2020 Oct 9].
- Das, Gautam. (2014). Clinical Methods in Pain Medicine.
- DO ZM. Cervicogenic Headache Causes and Risk Factors [Internet]. Spine-health. [cited 2020 Oct 9]. Available from: https://www.spine-health.com/conditions/neck-pain/cervicogenic-headache-causes-and-risk-factors
- Bogduk N, Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol. 2009 Oct;8(10):959–68.
- Gobel H. 11.2.1 Cervicogenic headache [Internet]. ICHD-3 Beta The International Classification of Headache Disorders 3rd edition (Beta version). [cited 2020 Oct 9]. Available from: https://beta.ichd-3.org/11-headache-or-facial-pain-attributed-to-disorder-of-the-cranium-neck-eyes-ears-nose-sinuses-teeth-mouth-or-other-facial-or-cervical-structure/11-2-headache-attributed-to-disorder-of-the-neck/11-2-1-cervicogenic-headache/
- Jull GA, Stanton WR. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalalgia Int J Headache. 2005 Feb;25(2):101–8.
- Fritz JM, Brennan GP. Preliminary examination of a proposed treatment-based classification system for patients receiving physical therapy interventions for neck pain. Phys Ther. 2007 May;87(5):513–24.
- Cleland JA, Mintken PE, Carpenter K, Fritz JM, Glynn P, Whitman J, et al. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multi-center randomized clinical trial. Phys Ther. 2010 Sep;90(9):1239–50.
- Luedtke K, Allers A, Schulte LH, May A. Efficacy of interventions used by physiotherapists for patients with headache and migraine-systematic review and meta-analysis. Cephalalgia Int J Headache. 2016 Apr;36(5):474–92.
- Biondi DM. Cervicogenic Headache: A Review of Diagnostic and Treatment Strategies. J Am Osteopath Assoc. 2005 Apr 1;105(4_suppl):16S-22S.
- Toby M. Hall, MSc, Kathy Briffa, PhD, Diana Hopper, PhD, and Kim W. Robinson, BSc. The relationship between cervicogenic headache and impairment determined by the flexion-rotation test. Journal of Manipulative and Physiological Therapeutics 2010; Volume 33: Number 9.


